Rhinology/Allergy
(1220) Mucormycosis Due to Apophysomyces: A Rare Case of Invasive Fungal Sinusitis in an Immunocompetent Individual
Monday, September 30, 2024
12:00 PM - 1:00 PM EDT
Has Audio
Disclosure(s):
Emily C. Newstrom, MD, MS: No relevant relationships to disclose.
Tran Locke, MD: No relevant relationships to disclose.
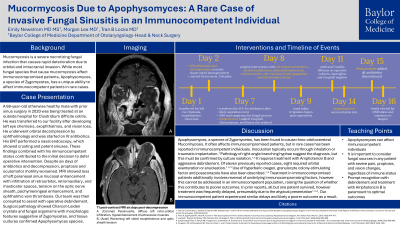
Introduction: Mucormycosis is a severe fungal infection that causes rapid deterioration with orbital and intracranial invasion. While most common in the immunocompromised, we present a case of mucormycosis due to Apophysomyces, a Zygomycetes species that uniquely affects immunocompetent patients.
Methods: A 69-year-old male with prior sinus surgery in 2020 presented from an outside hospital with left eye chemosis, exophthalmos, and vision loss. He underwent orbitotomy by ophthalmology and necrotic tissue was noted. His ENT deferred surgery as nasal endoscopy showed patent sinuses. Despite 6 days of IV antibiotics, he proptosis and oculomotor motility worsened. MRI showed loss of left paranasal sinus mucosal enhancement with infiltration of retroorbital, retromaxillary, and masticator fat, tension on the optic nerve sheath, pachymeningeal enhancement, and ophthalmic vein thrombosis. Amphotericin B was initiated and he went to OR with ophthalmology and our ENT team for left orbital exenteration, medial maxillectomy, sphenoethmoidectomy, turbinectomies, and pterygopalatine and infratemporal fossa debridement. Path showed Charcot-Leiden crystals and fungal organisms indicative of Apophysomyces species. Unfortunately, he developed right eye pain, vision loss, and palatal necrosis suggestive of intracranial extension via cavernous sinus. Given grave prognosis, patient and family opted for hospice.
Results: This patient developed rapidly progressive mucormycosis with few predisposing factors. He has no history of diabetes, immunosuppression, or trauma. No fungal elements were seen after prior sinus surgery. Limited reports describe Apophysomyces as a cause of mucormycosis in immunocompentent individuals. Prompt recognition with debridement and Amphotericin B is paramount to optimal outcomes. This patient likely experienced delays due to lack of immunocompromise.
Conclusions: This case contributes to understanding of Apophysomyces clinical manifestations and emphasizes the need to consider fungal sources for any patient with severe pain, proptosis, and vision changes, regardless of immune status.

Emily C. Newstrom, MD, MS
Resident Physician
Baylor College of Medicine
Houston, Texas, United States
Tran Locke, MD
Assistant Professor
Baylor College of Medicine
Houston, Texas, United States