Care Equity, Quality, and Safety
(0248) Race, Ethnic, and Gender Disparities in Papillary Thyroid Cancer Clinical Trials
Monday, September 30, 2024
12:00 PM - 1:00 PM EDT
Has Audio
Disclosure(s):
Michelle Sharon Klausner: No relevant relationships to disclose.
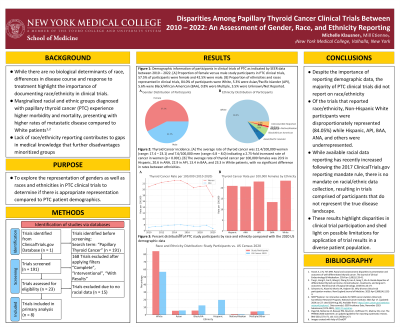
Introduction: Differences in disease course and treatment response highlight the importance of demographic representation in clinical studies. Marginalized groups diagnosed with papillary thyroid cancer (PTC) experience higher morbidity and mortality, yet their inclusion in clinical trials remains limited. This study aims to examine the demographic data in PTC randomized clinical trials (RCTs) between 2010-2022 to explore disparities in representation.
Methods: The National Library of Medicine’s ClinicalTrials.gov was used to search for RCTs pertaining to PTC. The search term “Papillary Thyroid Cancer” (n = 191) was used. Trials completed in the US were screened using the filters “Complete,” “Interventional,” and “With Results” (n = 23). Trials including race, ethnicity and sex demographic data were included in the secondary analysis (n = 8). National incidence data on PTC was extrapolated using the National Cancer Institute SEER Program.
Results: Of the clinical trials analyzed, 52.3% of participants were women and 47.7% were men. Between 2010-2020, the average rate of thyroid cancer per 100,000 was 21.4 in women (range 17.4 – 23.1), and 7.6 in men (range 6.8 – 8.0), indicating a 2.75-fold higher rate of cancer in women (p < 0.001). Chi-square analysis comparing women in the RCTs to women diagnosed with cancer in SEER showed women significantly underrepresented in the RCTs (p < 0.001). We found 84% of subjects were White, 5.3% Asian/Pacific Islander (API), 5.6% Black/African American (BAA), 0% Hispanic, 0.8% American Native/Alaskan (ANA), 0.8% multiracial, and 3.5% Unknown.
Conclusions: Though women made up most of research participants, they were significantly underrepresented compared to the prevalence of PTC (per SEER data) in women versus men. Over half of PTC RCTs did not report race, resulting in critical data being missed. Of the RCTs that reported race, White participants were disproportionately represented (84.05%) while Hispanic, API, BAA, and ANA were underrepresented, revealing disparities in clinical trial participation and potential limitations in applicability of results for diverse patient populations.

Michelle Sharon Klausner
Medical Student
New York Medical College
Valhalla, New York, United States- ME
Mill Etienne
New York Medical College
Valhalla, New York, United States